For many people, nasal congestion is a long-term battle. Others find certain triggers that bring it on. For example, you guessed it – spring. And extending on nasal congestion, some people go on to get “sinusitis”. Of course, it goes without saying that the ears and throat can get wrapped up in this whole facial conundrum. So what is this all about?
Let’s take a quick tour…
The nose: As well as providing the sense of smell, some other key functions of the nose are:
- It aids in the sense of taste
- It humidifies the air we breathe in. In fact, it plays a key role in this
- It warms and filters the air we breathe in
So when we have dysfunction of the nose, we can lose our sense of taste as well as smell and we can also go on to exacerbate other downstream respiratory problems, such as asthma.
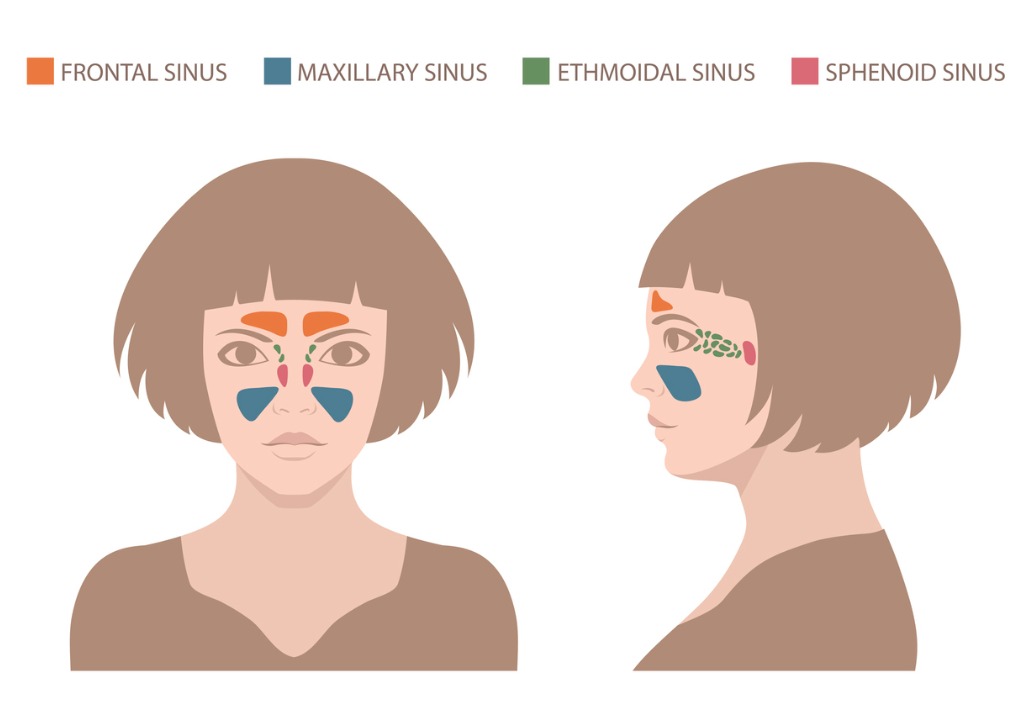
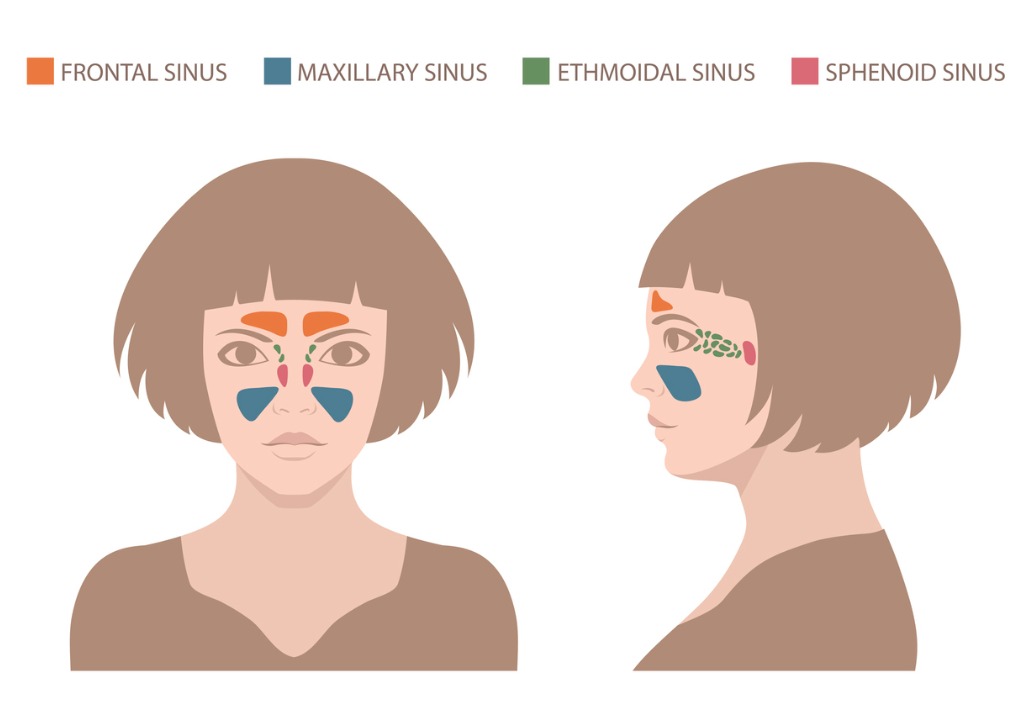
The sinuses: The sinuses are hollowed areas in the facial skeleton. There are four pairs of “paranasal” sinuses to be sure. These are:
- Frontal sinuses – in the forehead
- Maxillary sinuses – in the cheeks
- Ethmoid sinuses – beside the upper nose, between your eyes
- Sphenoid sinuses – behind the nose
No one really knows the purpose of these “sinuses” except that it is hypothesised that they may have a role to either make the skull lighter in weight or help your voice resonate. At any rate, they have a lining which, like most biological linings and internal surfaces, produces a fluid. This fluid needs to drain. Indeed, by virtue of the fact that they are air filled cavities, the sinuses need draining outlets to allow the pressure to equalise with the surrounding environment.
The ears: the ears are made up of three main compartments:
- The outer ear which is external to the ear drum
- The middle ear – which is the segment immediately deep to the ear drum. Here there are three small bones which transmit any sound wave from the ear drum to the…
- Inner ear – which leads to the nerve that sends a message to your brain about sound as well as balance.
Now the middle ear is of interest to us here. Since the function of this part requires bones to vibrate, the chamber of the middle ear is filled with air. Like the paranasal sinuses, it needs to ventilate. In this case, it does so via a natural ventilation pipe/tube, called the eustachian tube, that opens at the back of the nose in an area of the throat aptly described as the “nasopharynx”.
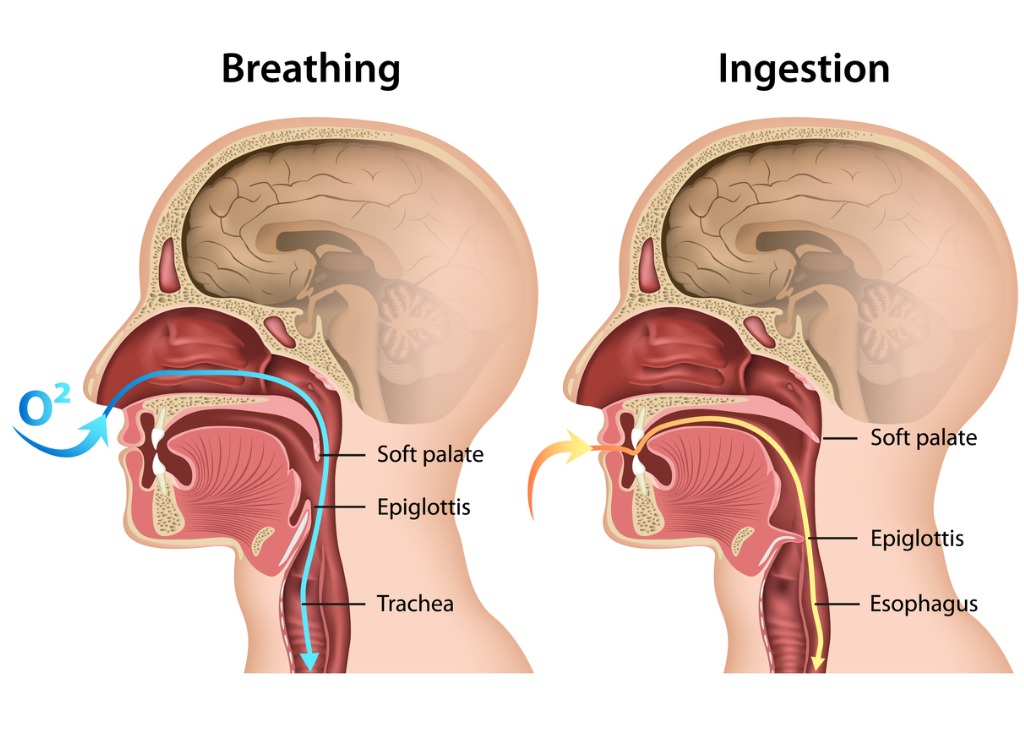
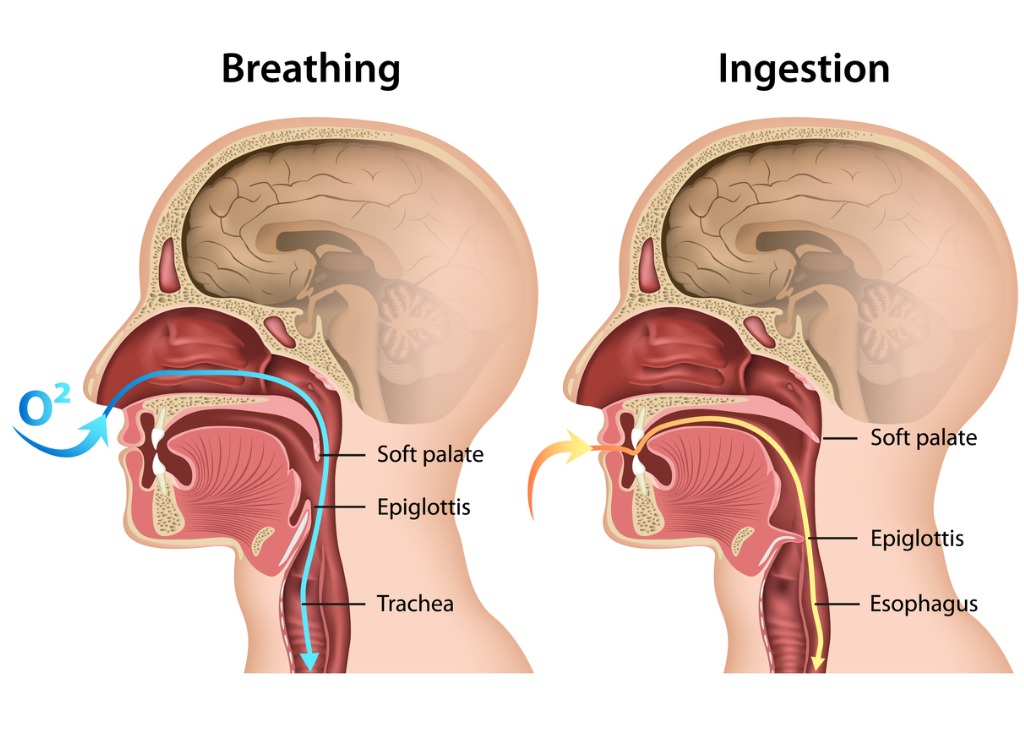
The throat: The throat or oro-pharynx as it is scientifically known has a dual job of transferring air as well as food and fluids. These things go down a common path until a bifurcation occurs, separating the throat into the wind pipe (trachea) and gullet (oesophagus). The entrance to this force is ingeniously guarded by a valve called the epiglottis, such that when you eat or drink, the epiglottis automatically shuts off the wind pipe. Yet when you inhale air, the epiglottis allows that air to rightfully and preferentially enter the wind pipe. Cool hey. Keep in mind also that at the top of the wind pipe are the vocal chords which are muscles and cartilage that allow you to talk. When you have lots of phlegm and mucus dripping down from the back of your nose, down your throat, eventually that phlegm tends to accumulate around and irritate your throat and vocal cords, causing you to cough and have an irritated throat. The problem is confounded at night when the forces of gravity cause more phlegm to drip down the back of your throat, and if your nose is blocked, you’ll mouth breathe all night. Mouth breathing tends to dry your throat, irritating it yet again. Therefore, often if you have nasal congestion and sinusitis, you’ll wake up the in morning with the need to clear your throat, and indeed a sore throat.
Putting this all together:
When a triggering factor (allergy, infection) causes inflammation in your nose, the openings to your sinuses can get blocked. At the same time, the presence of inflammation can likewise block the ventilation channels (eustachian tubes) that lead to your middle ears. The end result is that the pressure in these areas, your sinuses and middle ears can drop, and these chambers can fill with fluid. Indeed, at this time, you can feel “congested”. Adding to this picture, some people, particularly those with “allergy” tend to generate fleshy growths from the internal lining of their nose. These growths are called nasal polyps and the significance of them is that they can lead to a physical obstruction to the openings of the sinuses as well as causing difficulty to breathe through the nose itself. To make matters worse, all these blocked up passages are sitting ducks for bacterial infection to set in.
All in all, sinusitis is the presence of inflammation within the paranasal sinuses, brought about usually as a consequence of those sinuses being blocked within the nose. There can be a consequent degree of fluid collection in the sinuses which in turn can attract bacterial infection.
The question is – what to do?
The elements of what to do revolve around the cause in the first place. And the real issue is what causes the blockage of the opening of the sinuses within the nose? Those causes can be
- Infection – causing inflammation
- Allery – causing inflammation
- Anatomy – causing an ongoing fixed physical obstruction
With regard to infection, causing inflammation, note that this infection could be viral, as in the case of a simple “cold”, a viral upper respiratory tract infection to be precise. Or, it could be bacterial infection. How do you know which one you’ve got? How long you’ve had your problem for, and what other symptoms you have, can provide some indication. If you’ve only just been unwell for a few days to a week, and have a runny nose and cough, as well as facial “congestion” including sinus pain, then you’re likely to have viral sinusitis. If you’ve been unwell for more than ten days, have a high fever and your symptoms mainly comprise pain in your face and thicker phlegm or mucus from your nose that might be more colourful, they you’re more likely to have a bacterial infection.
Viral sinusitis is usually treated conservatively, with a view to avoid allowing it to develop into bacterial sinusitis. The way to do this is to unblock the sinus openings in the nose allowing these spaces to drain freely again. A part of this will occur spontaneously, as your body fights off and ultimately eliminates the virus and inflammation subsides. The other things you can do are:
- Drink lots of water so no part of your face and therefore internal nose are dehydrated, since dehydration will only make blockages greater and more likely to occur. In general warm fluids are better than those that are too cold since they can be a bit abrasive.
- Keep eating and drinking (again). This all helps you recover by providing you energy, but it also in this case, serves the purpose of keeping your face moving and in doing so, helps keep things “flowing”. If you don’t open your mouth much and keep rather still, whatever is blocked, is more likely to stay blocked. Stasis. The more you can keep your face moving, by talking and eating and drinking, the better. It’s worthwhile mentioning here that eating fruits with vitamin c and citric acid at this time, are particularly beneficial since these helpful elements with douse the back of your throat with all sorts of natural goodies that will help you recover. The local action of fruit, on your throat as it is eaten and swallowed, trumps the potential benefit of consuming vitamins which have a more indirect route to help, through your blood, in my opinion.
- Steam inhalation. This is used to humidify air and soothe physically stuck/blocked sinus openings in your nose. The classic way to do this is to get boiling water, add a little eucalyptus oil or Vicks, cover your head with the towel and sniff away. Be careful not too scold yourself in the process! Steam inhalation does work.
- Get a little bit of sunshine… it does help to activate your immune system!
- Take a break. When you’re unwell, it’s great to push through things to a degree with paracetamol and everything else that lets you soldier on. But don’t go too far, you’ll simply weaken your body, hampering it’s efforts to fight off whatever you’re fighting off and recover. Now is not the time to burn the midnight oil. When you’re unwell, it is time to slow down a notch, look after yourself which includes giving yourself enough time to destress and get your best sleep. Sounds simple I know, but would remiss of me not to at least mention here!
And now for the medical bit…
- Antibiotics. If you’ve had sinusitis for over a week, or if you’re prone to having stubborn bouts, you may have a bacterial infection within your nasal passages and sinuses and it’s worthwhile considering antibiotics. Antibiotics will in this case fight bacterial infection, and in doing so, help resolve the culprit inflammation causing blockage. Usual antibiotic choices include roxithromycin or amoxicillin. Since sinusitis is stubborn, you should take them for 10 days minimum. And, if after 5 days, you’re not improving at all, you may consider changing the antibiotic to something stronger such as amoxicillin/clavulanic acid (“Augmentin”).
- Prednisolone. Once again, if you can’t get over things naturally after about a week to 10 days, then you may find benefit from taking prednisolone, a steroid tablet. Steroids have a strong anti-inflammatory effect. They are typically taken for the first five days whilst you are taking antibiotics, as an adjunct.
- Nasal steroid spray. If things aren’t “too bad” and especially if your problem is thought to be related to allergy, a nasal steroid spray (such as Nasonex or Rhinocort) may be used to decrease the inflammation specifically in your nose. This can be particularly helpful for patients found to have nasal polyps as discussed earlier, since they reduce the size of these growths. Nasal steroid sprays are also particularly helpful for blocked eustachian tubes since the spray gets ideally right to the back of the nose, targeting that area. Be careful about your technique when using such a spray, because it’s not quite like a tablet that ends up in the right place rather automatically. A nasal steroid spray needs to remain in the back of your nose. If you inhale too aggressively whilst using it, you’ll taste it in your throat… and that means its gone beyond your nose!
- Antihistamines. These tablets are used decrease the production and release in your body of histamine. Histamine is part of the inflammatory response of your body which is particularly escalated during allergic reactions. Antihistamines, as the name suggests, decrease histamine and therefore reduce the symptoms of allergy which may be particularly present during spring for those who get hay fever. At a nasal level, antihistamines, by decreasing histamine and therefore inflammation, may help unblock the openings of the sinuses within the nose.
- Surgery: If all else fails, and sinusitis just happens too often or too severely, you may consider talking to an ear nose and throat (ENT) surgeon about what can be done. Before this, you should have a CT scan of your facial sinuses, to demonstrate the extent of things. An ENT surgeon will be able to look in your nose, in their rooms, with a special camera, a flexible nasendoscope and see things for themselves all the way down to your throat. Surgery is aimed to increase the calibre of the sinus openings, remove any polyps that may be present, and straighten the middle part of your nose, your septum, that at times can be crooked, leading to blockage of one nostril more than the other.
Well there you have it, a quick, yet hopefully sufficiently detailed explanation of all things sinusitis. Hopefully it helps you this spring smell the roses and breathe a little bit easier.