The digital stethoscope innovation has brought about significant advancements in medical auscultation. Among the leading contenders, the Thinklabs One and the 3M Littmann CORE stand out for their innovative features and enhanced sound quality. These devices offer a departure from traditional analog stethoscopes, incorporating digital technology to improve accuracy, versatility and user experience.
This comparative analysis will delve into the key features, strengths and weaknesses of each model, helping healthcare professionals make informed decisions about their digital stethoscope needs.
Amplification and Sound Quality

- Thinklabs One: Known for its unparalleled sound amplification, the Thinklabs One can amplify sound up to 100x, making it the loudest stethoscope in the world. It is particularly noted for its bass response, offering sound clarity even at low frequencies. While not explicitly mentioned as having active noise cancellation, its high amplification and design likely contribute to reducing background noise.
- 3M Littmann CORE: In comparison, the Littmann CORE offers 40x amplification, which is less than the Thinklabs One. However, it compensates with active noise cancellation, which filters out unwanted background sounds to deliver clearer, focused auscultation. Littmann’s device is designed to toggle between analog and digital modes, giving users the option to switch based on the listening scenario.
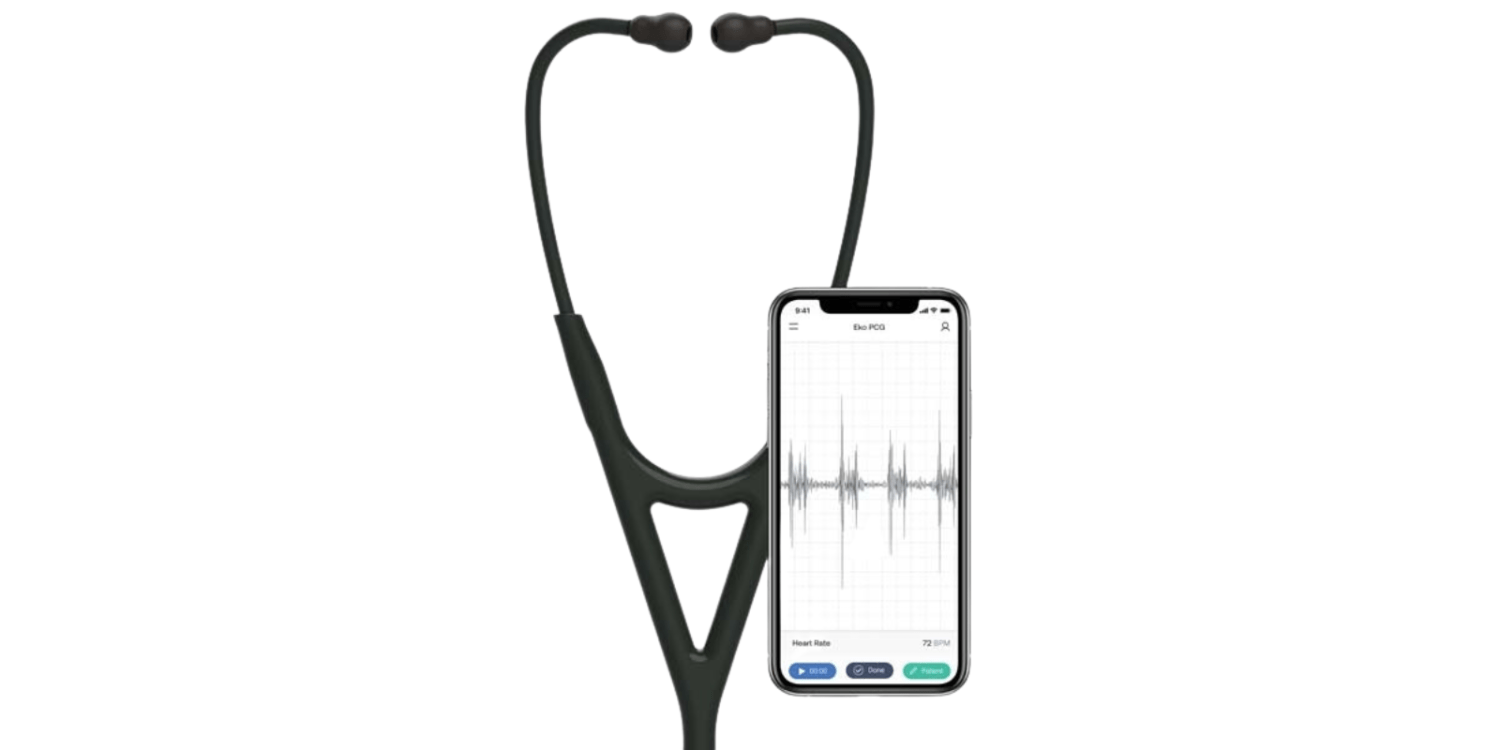
Digital Capabilities and Software Integration
- Thinklabs One: The Thinklabs One is designed with precision filtering, allowing users to switch between multiple filter options or listen to completely unfiltered sounds. It integrates with most videoconferencing and telemedicine systems, making it highly useful for remote consultations. Recording, saving and sharing of sound can be achieved via the Thinklabs Wave App. A similar application called eMurmur can be used for a cost.

- 3M Littmann CORE: Littmann’s CORE connects to Eko software which allows users to visualise, record and share heart sound waveforms. Additionally, it can store annotated recordings (15, 30, 60 or 120 seconds) in a secure cloud-based dashboard. It also offers AI integration (available separately) for detecting heart murmurs, a feature that provides clinicians with added diagnostic confidence.
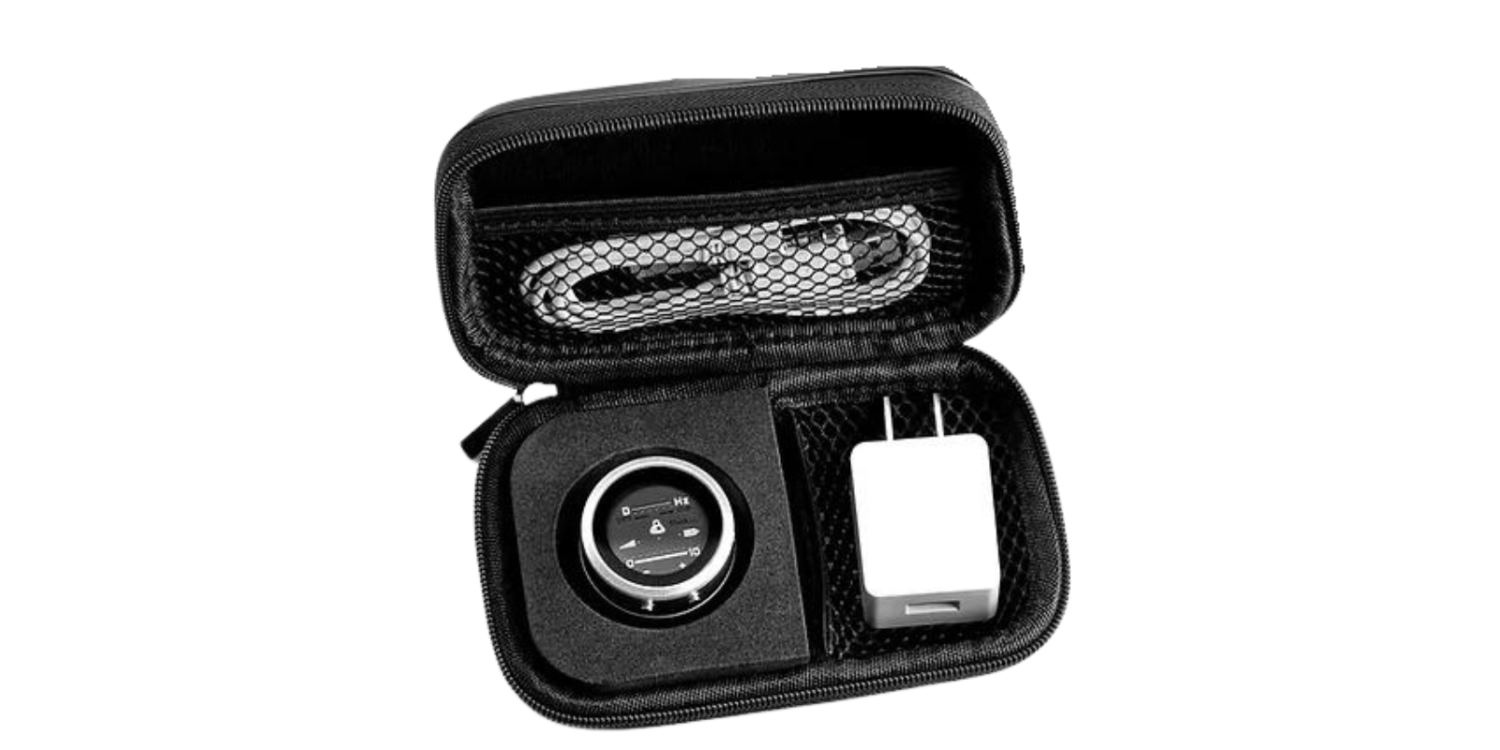
Battery and Power Management
- Thinklabs One: This model comes equipped with a rechargeable Lithium-ion battery. There’s no need to frequently replace batteries, making it practical for long, continuous use.
- 3M Littmann CORE: The Littmann CORE does not specify the battery life but emphasises its analog mode provides a backup listening option even if the digital battery is depleted.
Comfort and Design

- Thinklabs One: The Thinklabs One breaks away from traditional stethoscope design, featuring a compact, tubeless design. Instead of traditional binaurals, users can plug in any high-quality headphones via a 3.5mm jack. This allows for greater personalisation of listening devices.

- 3M Littmann CORE: Littmann maintains a more conventional stethoscope design with a dual-sided tunable chestpiece. Its soft-sealing ear tips are designed for comfort, providing an excellent acoustic seal, which improves sound isolation during auscultation. The chestpiece is made from high-polish materials, adding a professional aesthetic.
Versatility and Use Cases
- Thinklabs One: Its versatility is highlighted through applications in telemedicine, clinical practice and education. Its loud amplification also makes it suitable for healthcare professionals with hearing impairments.
- 3M Littmann CORE: The Littmann CORE, whilst also versatile, focuses heavily on diagnostic precision with features like tunable diaphragms for both adult and paediatric use. Its integration with the Eko software allows it to be used for disease monitoring, education and collaborative diagnosis, especially in more sophisticated medical settings.
Special Features

- Thinklabs One: The One boasts “plug-and-practice” functionality, where users can simply connect and use their preferred headphones. It also comes with a storage pouch, charger and specialised bass-optimised earbuds, making it a high-fidelity solution for listening to heart sounds. Thinklabs emphasises its sound engineering expertise, branding itself as a revolutionary product in medicine.

- 3M Littmann CORE: The Littmann CORE is marketed as a next-generation diagnostic tool, with advanced digital capabilities like waveform visualisation and AI assistance for murmur detection. It also includes noise cancellation and a tunable diaphragm, enhancing its accuracy during different medical assessments.
Pricing & Warranty:
Thinklabs One: $499 – 2 Years Warranty
3M Littmann CORE: Starting from $619 – 2 Years Warranty
Conclusion
Both the Thinklabs One and 3M Littmann CORE represent significant advancements in digital auscultation, though they serve different user needs.
Thinklabs One: Ideal for those seeking maximum sound amplification and versatility, especially for telemedicine, education, and those with hearing impairments. Its compact, headphone-based design offers a modern, flexible alternative to traditional stethoscopes.
3M Littmann CORE: Tailored for healthcare professionals who value precision and digital integration, particularly in diagnostic settings. Its connection with Eko software and AI capabilities offer a more sophisticated, tech-enhanced experience for disease monitoring and collaboration.