6 lessons I’ve learned working in healthcare during the pandemic:
1. When we look back on COVID-19 in the future, the direct health impact may not be what we remember most. Indirect effects on health, as a result of delayed routine and preventive care, overstressed healthcare systems, and the increased mental-health
2. People who were part of a community during the pandemic realised the importance of human connection, and those who didn’t have that kind of support realised they need it. Many of us have become aware of how much we need other people—many managed to maintain their social connections, even if they had to use technology to keep in touch.
3. While everyone’s situation is different (and some people have experienced tremendous difficulties), many have seen that it’s possible to be resilient in a crisis. People practised self-care in a multitude of ways during the pandemic as they were forced to adjust to new work schedules, change their gym routines, and cut back on socialising. Many started seeking out new strategies to counter the stress.
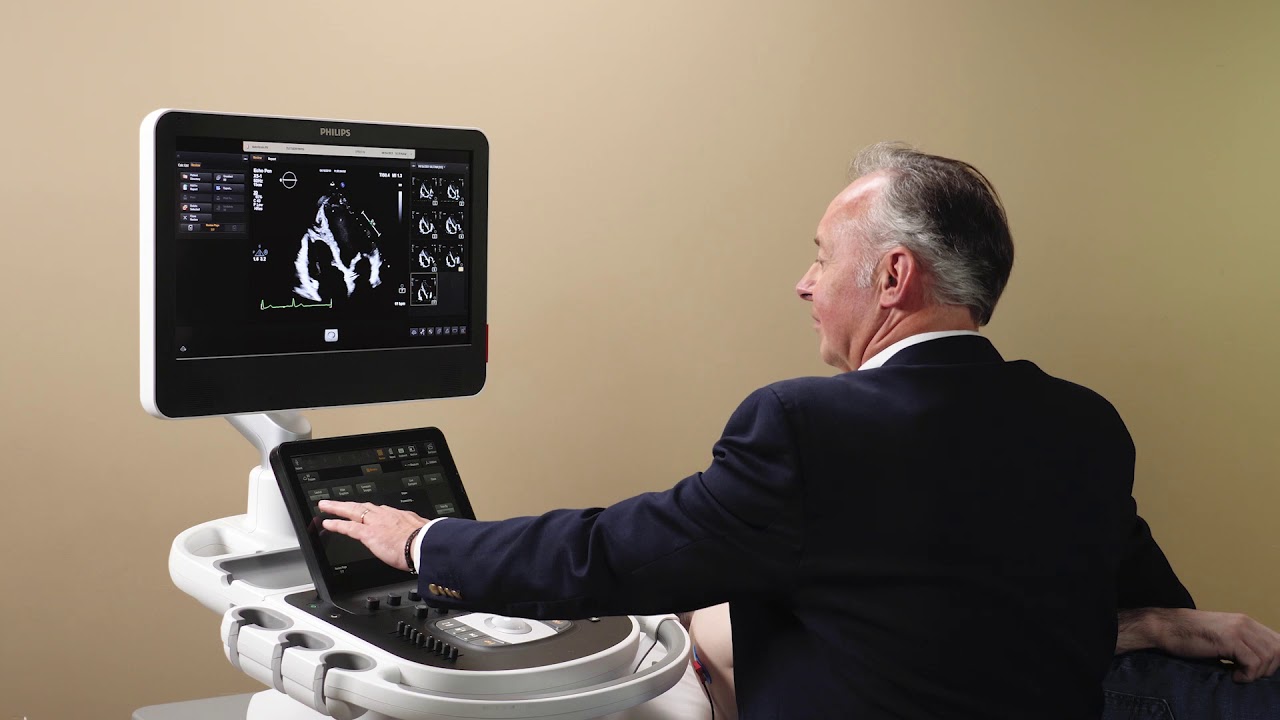
4. The number of virtual doctor’s appointments boomed since the pandemic began. Doctors and patients who used telehealth found it can work well for certain appointments. While there are still problems for which you need to see a doctor in person, the pandemic introduced a new urgency to what had been a gradual switchover to platforms like Zoom for remote patient visits.
5. People like health a lot more than they like healthcare. This is fine, keeping people healthy — and keeping them out of clinics — is the best and least expensive way to improve people’s health. Connecting patients with the resources and preventative health programs they need outside the clinic helped many stay healthy.
6. Importance of integrating mental health care and primary care. Mental health is another problem that was bad before and now is worse. Atticus Health integrated mental health services into primary care clinics, so our GPs and mental health professionals could collaborate to meet a patient’s physical and mental needs. Our GPs ask screening questions that help them focus on prevention and early diagnosis, and if patients needed further help, it’s easy to access our mental health social worker, either face to face or via Zoom (Telehealth).
Brett Thiedeman